Bladder pain syndrome
Bladder pain syndrome often results in doctors using the process of elimination to rule out the threat of underlying diseases and illness such as urinary tract infections before making the diagnosis.
What is interstitial cystitis?

Medically the term interstitial has different meanings. In this context it refers to the connective and fibrous tissues of the organs in our body. The word cystitis refers to inflammation of the bladder usually caused by a urinary tract infection.
So interstitial cystitis is the inflammation of the connective tissue in the bladder wall but without an infection or another reason for it. This feels very similar to a urinary tract infection, i.e. the need to urinate constantly, and when you do it really hurts. That’s why it’s called a syndrome – because it is complex and not really understood.
Inflammation is how your immune system protects itself against illness, infection, injury and invaders called pathogens. This inflammation causes microscopic tears and lesions which your body repairs. This in turn makes scar tissue. Constant inflammation creates more scar tissue in and on the bladder wall. Over time, the bladder wall starts to harden and thicken, losing its elasticity.
Your bladder’s job is to work with your kidneys to remove toxins and excess fluids from your body. As a form of reservoir, its function is to store the liquid that your kidneys filter out. It’s designed to expand and contract as it collects discarded fluids and toxins before they are eliminated as urine. On average, we should be urinating between six to eight times a day and once during the night.
For some people, the lining of the bladder wall becomes inflamed, irritated and scarred. This means that people with interstitial cystitis get hard, stiff bladders with a low capacity to store urine because their bladder wall becomes inflexible and oversensitive to their urine for no reason.
In fact, it may hurt to expand and contract so much that sleep is negatively affected due to trying to avoid the pain and discomfort of holding it in. It impacts their lives in many other ways.
About 5% of people with this syndrome also develop ulcers on their bladders eventually. It tends to get more noticeable during perimenopause for women.
What are the signs and symptoms of interstitial cystitis?

Symptoms vary from person to person. Flare-ups might last for six weeks or longer before subsiding. They may be constant and present all the time for some people or they may be episodic for others. They may be mild in some cases and debilitating in others.
About 90% of sufferers are women and it is said to affect between 3 to 6% of the female population. It also impacts men who are often misdiagnosed as having chronic prostatitis which is an infection in the prostate gland. Onset typically starts from around the mid-30s and the risk of getting it increases with age. However, it can start at any age.
Typical symptoms are felt in the pelvic region including the lower back, genitalia and the area just behind the belly button. They tend to include:
- Pain, either a mild throb or sharp shooting stabs, as the bladder begins to fill up.
- Needing to urinate frequently, particularly during the day but also at night causing sleep disruption.
- A sense of urgency and desperately needing to go even after having just been.
- In some cases, pain when urinating especially a burning sensation in the urethra.
- Pain or discomfort during and just after sexual intercourse.
- Tenderness and a feeling of pressure around the lower belly.
- Symptoms tend to get worse during times of stress and when anxious.
What causes interstitial cystitis?
Experts are significantly challenged to find a singular cause for bladder pain syndrome. Researchers believe that it is triggered by an initial damage to the bladder lining that results in making the nerves raw and sensitive.
Latest research suggests that people with interstitial cystitis produce a certain type of amino acid that makes the bladder’s nerves sensitive to its own urine, because it prevents the bladder wall from healing itself.
Likely causes include:
- Autoimmune disorders – this is when your immune system attacks itself. There are about 80 different types of autoimmune disorders, they all lead to chronic inflammation throughout the body including the lining of the bladder wall.
- Any type of trauma that might have caused scar tissue to the lining of the bladder wall.
- Recurring urinary tract infections in the past.
- Inflammation in other areas of the body.
- Problems with the muscles of the pelvic floor. These may have been caused by natural childbirth, chronic constipation, obesity, pregnancy and prostate cancer surgery which have been shown to weaken these muscles.
- A pH imbalance especially high levels of acid in the body might irritate the lining of the bladder wall.
- Spinal injury or irritation to the nervous system or the nerves that work with the urinary system may lead to the ongoing sensation of pain.
- An imbalance in the microbiome of the gut. Interstitial cystitis sufferers are 100 times more likely to have irritable bowel syndrome.
- Frequent cases of distention or being unable to urinate for long periods of time.
- Regularly being dehydrated and not drinking enough good quality water.
How is interstitial cystitis diagnosed?

This syndrome is diagnosed through a process of elimination. It needs to be done by a doctor to rule out the possibility of other diseases for the pain such as urinary tract infections. There could be other underlying causes too such as kidney stones or issues with the gut, prostatitis in men or ovarian issues such as endometriosis in women.
The severity of the symptoms is rated on an index called the O’Leary-Sant Symptom Index, also known as the Interstitial Cystitis Symptom Index (ICSI). The four main symptoms according to this index are bladder pain, urgency, frequency, and nocturia (frequent nighttime urination).
These are some of the common types of tests that are conducted before a definitive diagnosis is reached:
- Urine Analysis – a urine sample is tested for bacteria or other cultures caused by viruses, yeasts, or fungi, this is usually the first step.
- Ultrasound – also safe and non-invasive, this test allows the doctor to see how much urine is still left in the bladder after you have urinated.
- Cystoscopy – inserting a specialised camera into the bladder to check whether you have lesions, scar tissue, growths, tumours or anything out of the ordinary in your bladder.
- Urodynamic Evaluation - also known as bladder stretching which involves filling your bladder and then emptying it again under anaesthetic to test its capacity, pressure, and its functioning.
- Biopsy – checking the actual tissue in various parts of the urinary system for abnormalities.
What are the treatment options for interstitial cystitis?
There is no formal cure for interstitial cystitis. Because the causes behind the syndrome are so varied, there isn’t a singular approach to treatment. Everyone responds differently.
Treatment is aimed at preventing flare-ups, reducing inflammation, managing the symptoms especially pain relief, and improving quality of life. Holistic approach is often recommended and includes:
Maintaining the pH balance of your body and your bladder
High levels of acidity in the body lead to higher levels of acidity in the urine. Although urine is naturally slightly acidic, when the entire system is too acidic, urine pH becomes excessively acidic. This often triggers a flare-up as it aggravates the lining of the bladder wall. Regulating your pH balance is vital to good health.
- It is important to drink at least 1.5 litres of filtered water throughout the day to help the body flush out toxins, avoid dehydration, keep the pH balance of your urine stable so that it doesn’t irritate the bladder, drinking sufficient water also helps to prevent the formation of kidney stones.
- Strive to maintain a well-balanced diet that reduces acidity in the body by introducing more whole foods, fresh fruit, and vegetables as well as raw nuts and seeds. Try to limit meat, dairy products, sugar, processed foods, refined carbohydrates, and limit alcohol intake. Be cautious of carbonated drinks, caffeine, citrus fruit, tomatoes, and spicy food.
Recommended treatment:
Provide bladder support to manage symptoms
Long-term anti-inflammatory and pain relief treatments that support the connective tissue.
Recommended treatments:
 |
A.Vogel Bladder Irritation Formula This homeopathic medicine is for the supportive treatment of irritable bladder conditions. The ingredients address frequent, uncomfortable or urgent urination, an overactive bladder and urinary discomfort associated with minor infections of the urinary tract. |
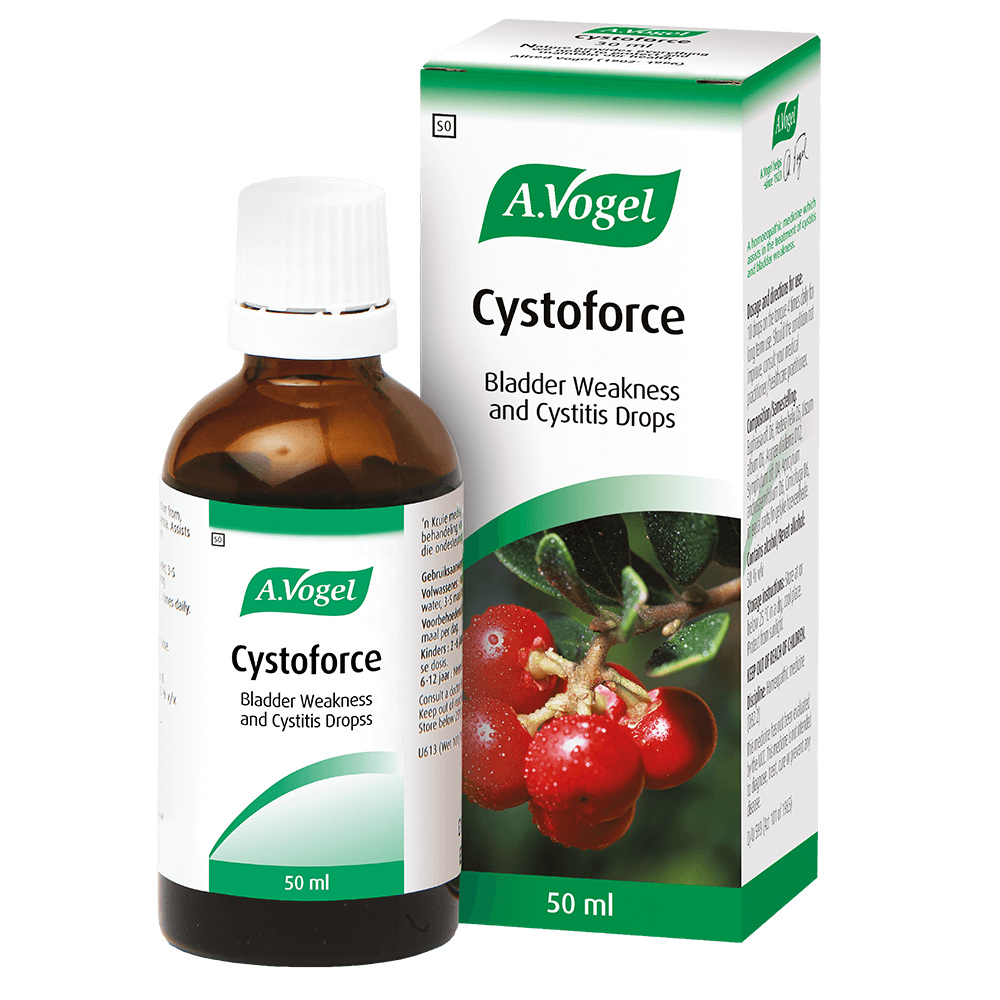 |
Better known as a tonic for the bladder, this herbal formulation is for the supportive treatment of bladder infections and bladder weakness. This Western Herbal medicinal product is used for the treatment of mild recurrent lower urinary tract infections such as burning sensations during urination and/or frequent urination. Although it is advised for use when the bladder is uncomfortable, it can be used long-term. It has anti-inflammatory properties. |
Bladder training
You may also want to consider looking into bladder training and specific exercises that strengthen the pelvic floor muscles. This involves:
- Training yourself to gradually increase the length of time between urinating. For example, if you need to urinate, time yourself. See whether you can hold it in for a few more seconds or even minutes before having to go again. Gradually increase the amount of time between trips. It helps to improve frequency.
- Locate your pelvic muscles. This can be done while urinating. Try to stop the flow mid-stream. Those are the muscles that need exercising. Squeeze and hold for 20 seconds and relax for 10 seconds while watching television, driving the car or reading a book. Repeat 15-30 times every day.
- Walking daily for half an hour and training your core are also shown to strengthen these muscles. Pilates is particularly good and strengthens the core. Doing Pilates twice a week will result in significant improvement.
Consult a certified homeopathic doctor
Homeopathic doctors may assist in prescribing specific remedies for you and your overactive and painful bladder. These medicines come without side effects and are safe to use with other medications.
And remember, it’s important to avoid getting bladder infections in the future. Prevention is always better than cure.
Parts of this article appeared on Living Naturally.
References:
- Treating interstitial cystitis or bladder pain syndrome naturally (2023) Living Naturally. Available at: https://livingnaturally.co.za/articles/general-healthcare/treating-interstitial-cystitis-or-bladder-pain-syndrome-naturally
- The Free Dictionary. Farlex. Available at: https://medical-dictionary.thefreedictionary.com/interstitial
- Rashid HH; Reeder JE; O'Connell MJ; Zhang CO; Messing EM; Keay SK; (no date) Interstitial cystitis antiproliferative factor (APF) as a cell-cycle modulator, BMC urology. U.S. National Library of Medicine. Available at: https://pubmed.ncbi.nlm.nih.gov/15068487/
- Treating interstitial cystitis (2017) Harvard Health. Available at: https://www.health.harvard.edu/diseases-and-conditions/treating-interstitial-cystitis/.
- Interstitial cystitis association (2023) Interstitial Cystitis Association |. Available at: https://www.ichelp.org
- Interstitial cystitis (2021) Mayo Clinic. Mayo Foundation for Medical Education and Research. Available at: https://www.mayoclinic.org/diseases-conditions/interstitial-cystitis/symptoms-causes/syc-20354357
- Interstitial cystitis: Symptoms, causes, and treatment (no date) Medical News Today. MediLexicon International. Available at: https://www.medicalnewstoday.com/articles/304366
- Yoshimura, N. and Chancellor, M.B. (2003) Neurophysiology of lower urinary tract function and dysfunction, Reviews in urology. U.S. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1502389/
- Diggs, C. et al. (2007) Assessing urgency in interstitial cystitis/painful bladder syndrome, Urology. U.S. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1855150/.
- Interstitial cystitis (painful bladder syndrome) - NIDDK (no date) National Institute of Diabetes and Digestive and Kidney Diseases. U.S. Department of Health and Human Services. Available at: https://www.niddk.nih.gov/health-information/urologic-diseases/interstitial-cystitis-painful-bladder-syndrome
- Interstitial cystitis (no date) What is Interstitial Cystitis(IC)/Bladder Pain Syndrome? - Urology Care Foundation. Available at: https://www.urologyhealth.org/urology-a-z/i/interstitial-cystitis
- Bladder training: What it is and how to do it (no date) Medical News Today. Available at: https://www.medicalnewstoday.com/articles/bladder-training#how-to-perform


